"Our integration with the Google Nest smart thermostats through Aidoo Pro represents an unprecedented leap forward for our industry."
- Antonio Mediato, founder and CEO of Airzone.
Healthcare organizations have relied on electronic medical records and electronic health records for decades. What started as a digital replacement for paper charts has now become the backbone of clinical operations, compliance, billing, and patient engagement. Yet many providers quietly admit the same thing. Their EMR or EHR system works, but it no longer works well.
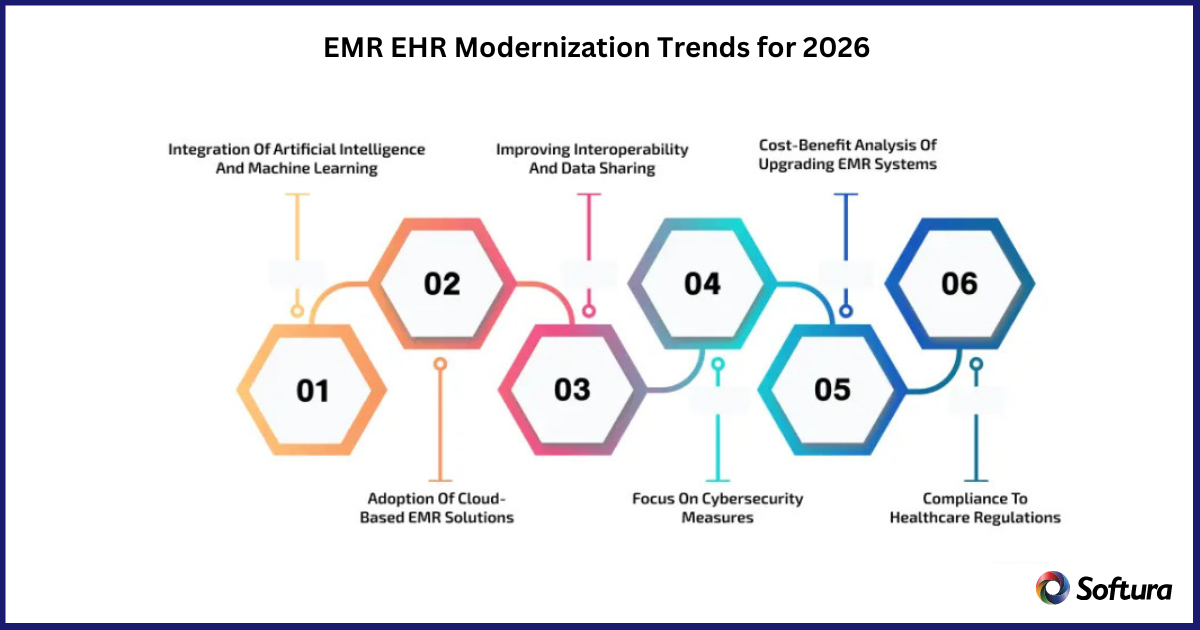
As healthcare moves into 2026, App modernization is no longer optional. It is becoming a strategic requirement driven by clinician burnout, patient expectations, regulatory pressure, cybersecurity risks, and the growing role of data in care delivery.
This article explores the most important EMR and EHR modernization trends shaping healthcare in 2026. It focuses on what providers actually need to know, not vendor hype or academic theory. The perspective reflects years of real world healthcare technology transformation and insights commonly shared by CIOs, CMIOs, and healthcare executives navigating modernization decisions today.
Most healthcare organizations are not running outdated systems because they want to. They are running them because replacing or modernizing core clinical platforms is complex, expensive, and disruptive.
However, several forces are converging in 2026 that make standing still riskier than moving forward.
Clinicians are overwhelmed by documentation burden. Patients expect digital experiences similar to other industries. Regulators demand better interoperability and data transparency. At the same time, legacy EMR and EHR platforms struggle to adapt without significant customization.
Healthcare leaders increasingly recognize that modernization does not always mean replacement. In many cases, it means rethinking how existing systems are extended, integrated, and optimized.
"Our integration with the Google Nest smart thermostats through Aidoo Pro represents an unprecedented leap forward for our industry."
- Antonio Mediato, founder and CEO of Airzone.
Traditionally, EMR and EHR platforms functioned as systems of record. They captured clinical data, stored it securely, and supported basic workflows.
In 2026, expectations are very different.
Modernized platforms are evolving into systems of intelligence. They do more than store data. They support clinical decision making, operational insight, and population health strategies.
This shift is driven by better analytics, AI assisted insights, and improved data access across care settings. Providers want systems that help answer questions, not just document encounters.
Executives often describe this transition as moving from digital filing cabinets to active clinical partners.
"By analyzing the data from our connected lights, devices and systems, our goal is to create additional value for our customers through data-enabled services that unlock new capabilities and experiences."
- Harsh Chitale, leader of Philips Lighting’s Professional Business.
Interoperability has been discussed for years, often with limited progress. In 2026, it becomes far more practical.
Regulatory pressure, standardized APIs, and cloud based architectures are finally reducing friction between systems. Providers increasingly expect their EMR or EHR to exchange data seamlessly with labs, imaging systems, payer platforms, and external providers.
Modernization efforts now prioritize clean data exchange rather than custom point to point integrations. This improves care coordination and reduces administrative overhead.
Interoperability is no longer framed as a compliance requirement. It is viewed as a care quality and efficiency enabler.
One of the most important modernization drivers in 2026 is clinician experience.
Physicians, nurses, and care teams are vocal about what slows them down. Excessive clicks, rigid workflows, and poor usability contribute directly to burnout.
Modernization trends focus on simplifying interfaces, reducing documentation burden, and aligning workflows with how clinicians actually work.
This includes better use of templates, voice enabled documentation, context aware forms, and role based interfaces. The goal is not to add features, but to remove friction.
Healthcare executives increasingly measure modernization success by clinician adoption and satisfaction, not just system uptime
Cloud adoption in healthcare has accelerated, and EMR and EHR platforms are following.
In 2026, cloud first architectures are becoming the default choice for modernization initiatives. They offer scalability, resilience, and faster innovation cycles compared to traditional on premises deployments.
Cloud based platforms also support better disaster recovery, remote access, and integration with advanced analytics and AI services.
Security concerns remain important, but cloud maturity and compliance frameworks have reached a level where many healthcare leaders see cloud as a safer option than aging internal infrastructure.
As EMR and EHR systems become more connected and intelligent, data governance becomes critical.
Healthcare providers are paying closer attention to data quality, access controls, auditability, and ownership. Poor data governance undermines clinical confidence and limits the value of analytics and AI.
App Modernization efforts increasingly include master data management, data stewardship models, and clearer policies around data use.
Trust in data is emerging as a foundational requirement for digital healthcare transformation.
Cybersecurity threats continue to rise across healthcare. Ransomware attacks, data breaches, and system outages carry serious clinical and financial consequences.
In 2026, security is no longer treated as an afterthought or add on. It is embedded into modernization design.
Modern EMR and EHR architectures emphasize zero trust principles, role based access, continuous monitoring, and regular security updates.
Healthcare leaders increasingly view modernization as an opportunity to reduce risk rather than introduce it.
AI is becoming more visible inside EMR and EHR environments, but its role remains focused and pragmatic.
Rather than replacing clinicians, AI supports them by highlighting relevant information, suggesting documentation, and identifying potential care gaps.
Examples include predictive alerts, clinical summarization, and automated coding assistance. These capabilities reduce cognitive load and improve consistency.
Successful organizations introduce AI gradually, ensuring transparency and clinician trust.
Despite progress, challenges remain.
Addressing these issues requires strong governance and shared ownership between IT and clinical stakeholders.
CIOs, CMIOs, and digital health leaders increasingly evaluate modernization through a strategic lens.
They focus on:
Modernization is treated as a continuous journey rather than a one time project.
EMR and EHR modernization has reached a point where incremental fixes are no longer sufficient.
Healthcare providers face rising expectations from patients, clinicians, regulators, and partners. Systems must support collaboration, insight, and adaptability.
Organizations that modernize thoughtfully position themselves to deliver better care with less friction.
EMR and EHR modernization in 2026 is not about chasing trends. It is about building systems that support clinicians, protect patients, and enable smarter decisions.
When modernization efforts focus on usability, interoperability, security, and trust, healthcare organizations gain more than technical upgrades. They gain resilience.
Connect with Softura to explore how EMR and EHR modernization can support better clinical experiences, stronger data foundations, and future ready healthcare operations.